The skin is the body’s largest organ, and it is made of multiple layers and has a diverse
range of functions. As it is our most external organ directly interacting with the
environment, it is the body’s first line of defense against external pathological factors.
The skin contains a variety of nerve endings that alert the body to react to heat and
cold, touch, pressure and tissue injury. It also helps to regulate water metabolism by
storing water and allowing evaporation through the sweat glands when bodily
temperature rises. It also stores lipids and absorbs oxygen in small amounts.
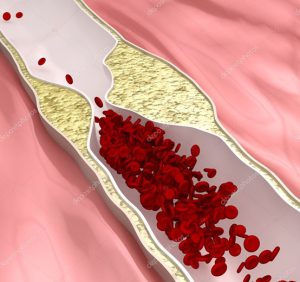
Although the skin has those specific purposes and functions, it also interconnects with
all the other bodily parts and particles, through nerves, chemical and physical
pathways, and most importantly – the blood. The blood is what nourishes the skin
from within, and grants the skin the chemical capability to perform its many tasks.
Therefore, the skin itself and its related disorders cannot be separated from the
function of the internal tissues and cells. Usually, a skin pathology erupts in a specific
area of the body, and this may seem as a mere local disorder. However, as the function
of the blood is to nourish cells and tissues and evacuate waste products, it stands to
reason that any pathology of the blood can also negatively affect the skin’s ability to
perform its functions. Through this interconnectedness between skin and blood, when
the skin develops a pathology, whether viral, bacterial or fungal, signs of the infection
should also come up in the blood tests. The way the blood test parameters indicate the
existence of the infection is beyond the scope of this article. However, it is mentioned
here, as it is crucial to realise that exposing the root causes of our skin issues requires
us to look deeper than just at the skin level.
The Human Skin is comprised of 2 main layers:
Epidermis – The epidermis is composed of the outermost layers of the skin. It forms a
protective barrier over the body’s surface, and is responsible for keeping water and
nutrients in the body, preventing external pathogens such as bacteria and viruses from
entering, as well as regulating body temperature.
Dermis – The dermis is the layer of skin beneath the epidermis consisting of
connective tissue. It protects the body from external pressure, as well as providing
elasticity. It contains nerve endings that provide the sense of touch, cold and heat, as
well as hair follicles, sweat glands, sebaceous glands, apocrine glands and lymphatic
vessels. Its blood vessels serve both the dermis and the epidermis.
The skin is connected to the inner bones, muscles, nerves and blood vessels through
another connective tissue layer called hypodermis or subcutaneous tissue.
Problems that appear on the skin are indeed sometimes limited to the skin.
However, in most cases a skin problem indicates an existing disorder that
affects the inner body. Consequently, the medical diagnosis should investigate
other possible inner diseases, when evaluating skin problems.
The fact that those who are most susceptible to skin
infections are immunocompromised is one of the ways to
establish the crucial interconnection between the skin
and the function of the internal bodily systems.
Although the skin is a rather “simple”-structured organ, the range of skin pathologies
is wide and can include all sorts of infectious, inflammatory, degenerative and/or
neoplasmic disorders.
Biochemically, a skin disease can be roughly associated with 3 major types of direct
pathogens:
1. Viral
2. Fungal
3. Bacterial
Viral – Many viral infections, such as measles, chickenpox, and rubella, cause rashes,
spots, or sores on the skin, as well as other symptoms. Viral skin lesions may be the
result of a direct viral replication effect, but also due to the bodily response to the
presence of the virus. In all of these cases, the viruses themselves are systemic
(throughout the body), often accompanied by other symptoms, such as fever and
headaches. Confirmation of a skin pathology labeled viral is usually pursued by
general lab diagnosis methods such as viral culture, microscopic examination, and/or
detection of viral antigens through blood tests. However, once diagnosed, an efficient
and thorough treatment must take into consideration the fact that the cutaneous
pathophysiology is a result of a deeper and more imbedded internal issue.
Fungal – Fungi usually make their homes in moist areas of the body where skin
surfaces meet – e.g. between the toes, in the genital area, or under the breasts. Fungal
skin infections are caused by yeasts (such as Candida) or dermatophytes, such as
Epidermophyton, Microsporum, and Trichophyton. A fungal infection is usually
accompanied by a red, irritated, or scaly rash in one of the commonly affected areas.
The diagnosis can be confirmed by scraping off a small amount of skin and having it
examined under a microscope or placed in a culture medium, where the specific
fungus can grow and be identified.
These pestering microorganisms infesting the skin are causing the irritating
symptoms, but they are not the sole cause for the infection. Sometimes they would
remain dormant, but a non-hygienic environment will cause the fungal organisms to
reproduce rapidly, leading to an infection. Simple measures in everyday life, such as
cleaning hands and feet, wearing clean, dry underwear and socks and raising the
hygiene standards of your body and surrounding environment, would go a long way
in preventing these infections. Yet, in order to efficiently treat the skin, one must
address the underlying cause for the body succumbing to the pathogen due to the
failure of the various levels of defense. Merely destroying the organism and not
addressing the root causes for its success to flourish will not guarantee prevention of
the infection from reappearing.
Bacterial – Humans are natural hosts for many bacterial species that colonize the skin
as normal flora. However, these bacteria can cause skin infections if they enter the
body through cuts, tears and open wounds in the skin or through poor hygiene.
Symptoms of a skin infection may include redness, swelling, pain, or pus. While
many bacterial skin infections are mild, in some people, a skin infection can lead to a
more serious and even life-threatening, invasive infection deeper within the body.
Staphylococcus aureus and Streptococcus pyogenes are infrequent resident flora, but
they account for a wide variety of bacterial suppurative skin diseases. Here too, the
severity of the infection and its effect on the internal organs and systems indicates the
level of weakness in the body’s immunity and defense mechanisms. The state of the
body’s immunity, and the root causes for its failure to protect the body, must be taken
into account in the treatment in order to prevent a reoccurrence of the infection.
To conclude, although skin lesions and diseases are externally apparent, there is a
need to diagnose the root causes of the skin pathology. These root causes run much
deeper than what meets the eye or is seen on the surface of the body, and the medical
investigation must turn to the internal body. The skin does not fulfill its functions
regardless of the internal parts of the body, and it depends on other bodily systems for
nourishment and sustenance. The body is comprised of brilliant systems working as a
whole, combining myriads of mechanisms into a single entity with a common
homeostatic goal. Skin lesions can provide some essential clues as to what went
wrong – e.g. failure of immunity and/or problem in the blood system. The failure of
these two systems indicate yet deeper possible root causes, which need to be further
investigated to go to the root of things, and offer an efficient and long-term treatment
results. Utilizing properly basic diagnostic tools, such as a comprehensive blood
work, can help discover those underlying causes, and take us closer to treating it at the
root.